Pelvic Visual Analog Scale (P-VAS)

Download the P-VAS Scale
Download Now
Introduction
Many healthcare professionals, including Pelvic Floor Therapists, Gynecologists, Urologists, Gastroenterologists, and exercise professionals are generally interested in the active and passive properties of the Pelvic Floor Muscles (PFM). The active properties or force generating capacity of the PFM can be seen as the strength while the passive properties or resistance to passive stretch can be seen as the tone or laxity, which can be used interchangeably.1 Both of these properties can be determined by assessing the vertical displacement of the PFM using a variety of digital examination methods.2,3 These examination methods are dependent on a practitioner’s assessment and have variable inter- and intra-rater reliability values. Thus far, there has not been a development of a subjective outcome measure to determine the “sense” of muscle strength and laxity a patient may feel. In order to subjectively determine a patient’s PFM strength and laxity, an analogue scale can be used. An analogue scale is often used in various types of research to measure the intensity or frequency of symptoms. For example, the Visual Analog Scale (VAS) of pain addresses the amount of pain that a patient feels across a continuum from none to an extreme amount of pain.4 From the patient’s perspective, this spectrum appears continuous and does not take discrete steps. For any practitioner who is interested in a patient’s self-perception of PFM qualities, an analog scale has been developed to allow a patient to determine their own judgment of PFM strength versus laxity as the quantifying measures.
Purpose
The purpose of the Pelvic Visual Analog Scale (P-VAS) is to provide a subjective tool for patients and practitioners to analyze a unidimensional vertical measure of both PFM strength and laxity. As the vertical displacement of PFM strength and laxity are perceived in the longitudinal axis of the body, a vertical analog scale can be used to relay information that is difficult to determine in the absence of a physical examination.
Definition of Tone
Muscle tone is defined as a muscle’s resistance to passive stretch during a resting state.5 As PFM tone is difficult to assess for a patient population without an examination or the use of equipment, we can rely on the patients subjective experience of strength and laxity in the vertical axis and how this correlates to resting PFM tone.
Structure, Orientation, and Response Options
Currently, the P-VAS can be measured vertically using a 4 point scale for both strength (positive values) and laxity (negative values), where 0 is the rest position which is located in the middle. There is a descriptive term located at each interval along the vertical line to help guide the patient about the level of intensity throughout the continuum.
The P-VAS has a simple vertical line of fixed length of 80mm. The ends of the scale are defined as the extreme limits of both strength (+y) and laxity (-y). The middle marks the rest position or 0 point. Each interval consists of 10mm for a total of 40mm in the positive direction for PFM strength (+y) and 40mm in the negative direction for PFM laxity (-y). A horizontal scale with a similar structure is not recommended.
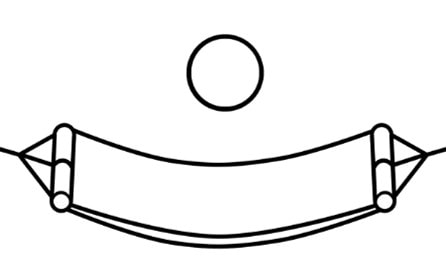
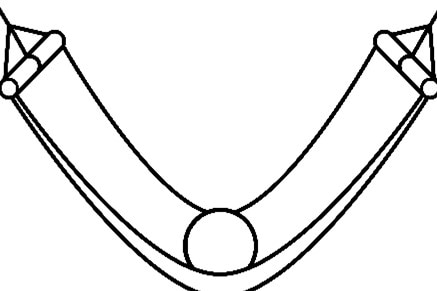
Accompanying the maximum and minimum ends of the scale and the resting point at 0, are images of a hammock and ball at different states. The ball is used to represent the level of strength and tone within the hammock. The 0 point represents the hammock or pelvic floor at rest, when there is no contraction of the PFM up or stretch down.
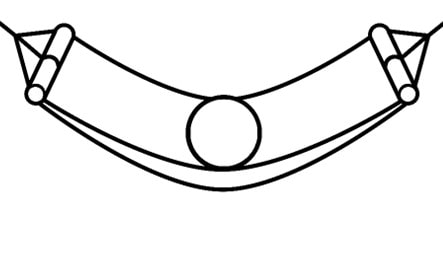
The maximum +y state indicates when the hammock is at its maximal height of tension, or when the tension in the hammock is high in order to throw the ball into the air.
The minimum -y state indicates when the hammock is at minimal height of tension, or when the ball is resting on the ground.
Measurements
There are 2 measures that are obtained in the P-VAS. The first measure or measure A is a patient’s perception of upward vertical movement of the PFM on activation and determines the patients force generating capacity. The scale has been set from 0 to 4 as very weak (1), weak (2) , strong (3) and very strong (4) in the positive direction.
The second measure or measure B is a patient’s perception of downward vertical movement of the PFM on stretch. This is a measure of laxity or tone during passive stretch. The scale has been set from 0 to 4 as very taut (1), taut (2), lax (3) and very lax (4) in the negative direction.
The third section allows both patient and practitioner to input A and B into a simple grid to correlate these values to the patient’s overall perception of resting pelvic floor tone. This grid requires the patient or practitioner to use the strength and laxity values and determine the coordinate in the grid where they intersect. Based on this intersection point, the PFM resting tone state can be determined. If the intersection point falls in the dark gray zone, the resting tone state will tend to be overactive. If the intersection point falls in the medium gray zone, the resting tone states will tend to be balanced or neutral. If the intersection point falls in the light gray zone, the resting tone will tend to be underactive. Note that dysfunction can occur with any of these three tonal states and there is no right or better answer. The information that is gained is how a patients perceives their PFM in terms of strength and laxity which may help determine the right course of therapy or treatment if dysfunction does exist.
Administration
The scale can be completed by patients themselves by reading the instructions and scoring themselves or by healthcare providers interested in a patients own perception of their strength and laxity
The patient marks on the line the point that they feel represents their perception of their current state of strength in the positive scale and laxity in the negative scale
The P-VAS score is determined by measuring in millimeters from the 0 point to the point that the patient marks in the positive and the negative directions for strength and laxity, respectively
The overall tendency of the resting tone of the pelvic floor can be correlated by intersecting the strength or A score with the laxity or B score
Scoring and Interpretation
Using a ruler, the score is determined by measuring the distance (mm) on the 80 mm line. To determine the strength value, measure between the rest point at 0 and the patient’s mark, providing a range of scores from 0mm to 40mm; higher score indicates greater perception of strength. For the determination of laxity, measure between the rest point at 0 and the patient’s mark, providing a range of scores from 0mm to -40mm; lower scores indicate greater perception of laxity.
The following descriptions accompany the varying levels of strength to calculate value A: very weak (0 to 10mm), weak (10 to 20 mm), strong (20 to 30 mm), and very strong (30 to 40 mm).
The following descriptions accompany the varying levels of laxity to calculate value B: very taut (0 to -10mm), taut (-10 to -20 mm), lax (-20 to -30 mm), and very lax (-30 to -40 mm).
Patients and/or practitioners may intersect the values from A and B on the grid to determine the pelvic floor resting tone. Depending on where these values intersect, the pelvic floor at rest may be overactive, balanced or underactive.
It is recommended that the scale be shown rather than read to the patient as the images and the ability to mark the y axis along the line require visual input.
Recall Period for items
The recall period is for the current state of pelvic floor and can be determined during the time of administration of the P-VAS.
Merits and Demerits
The P-VAS can be used to subjectively assess both female and male pelvic floor muscle strength and laxity with ease and without the need of a physical exam. This scale can be applied to a broad range of populations and settings.
Merits
- P-VAS is more sensitive to small changes than simple descriptive ordinal scales
- The scale can be used to determine a current state and compare it at a later time to detect change within individuals
- The P-VAS takes less than 2 minutes to complete and takes less than 1 minute for a practitioner to score
- No training is required other than the ability to use a ruler to measure distance to determine a score
- P-VAS can be assessed in all positions including standing, sitting and supine.
Demerits
- The assessment is subjective
- The P-VAS is administered as a paper and pencil measure and requires visual references regarding the hammock. Thus, it cannot be administered verbally or by phone.
- Caution is required when photocopying the scale as this may change the length of the 80mm line and also, the same alignment of scale should be used consistently within the same patient
- Obtaining the scale
The P-VAS is available in the public domain at no cost. The P-VAS is the property of Stroma Physical Therapy, LLC.
Psychometric Information
Method of development
The P-VAS was first conceived by Vinita Chandra Mody, PT in 2018 as she was attempting to determine the state of her patients’ pelvic floor environment prior to objective assessments. She would then attempt to see if there was a correlation between the patient’s perception and the digital pelvic floor muscle strength examination. She looked at the variety of scales that existed and realized that there was no subjective scale available to patients. She decided that resting pelvic muscle tone, as perceived in the vertical axis, was a critical determiner of function in Activities of Daily Living (ADL’s) and put efforts together to set up a scale that could be used by both patient and practitioners to determine qualities of strength and laxity as it correlates to resting pelvic muscle tone.
Acceptability
The P-VAS requires little training to administer and score and has been found to be acceptable to patients. However, patients with cognitive impairments, men, and women who have not had children demonstrate difficulty understanding and therefore completing the scale. Supervision during completion may minimize these errors.
Citations
1. Mary P FitzGerald, Kathryn L Burgio, Diane F Borello-France, Shawn A Menefee, Joseph Schaffer, Stephen Kraus, Veronica T Mallett, Yan Xu. Pelvic-Floor Strength in Women With Incontinence as Assessed by the Brink Scale, Physical Therapy, vol. 87, no. 10, 2007, pp. 1316–1324., https://doi.org/10.2522/ptj.20060073
2. Brink, Carol A., et al. “A Digital Test for Pelvic Muscle Strength in Older Women With Urinary Incontinence.” Nursing Research, vol. 38, no. 4, 1989, pp. 352–356.
3. Morin, Mélanie, et al. “Application of a New Method in the Study of Pelvic Floor Muscle Passive Properties in Continent Women.” Journal of Electromyography and Kinesiology, vol. 20, no. 5, 2010, pp. 795–803., doi:10.1016/j.jelekin.2009.10.004.
4. D. Gould et al. “Visual Analogue Scale (VAS).” Journal of Clinical Nursing, vol 10, 2001, pp. 697-706.
5. O’Sullivan, S. B. (2007). Examination of motor function: Motor control and motor learning. In S. B. O’Sullivan, & T. J. Schmitz (Eds), Physical rehabilitation (5th ed.) (pp. 233-234). Philadelphia, Pennsylvania: F. A. Davis Company.
6. Physics for Scientists and Engineers with Modern Physics, Section 5.7. Seventh Edition, Brooks/Cole Cengage Learning, 2008.
References
Aanestad,O., Flink, R. (1999) Urinary stress incontinence: a urodynamic and quantitative electromyographic study of the perineal muscles. Acta Obstet Gynecol Scand., 78: 245– 253.
Frawley, Helena C., et al. “Reliability of Pelvic Floor Muscle Strength Assessment Using Different Test Positions and Tools.” Neurology and Urodynamics, vol. 25, no. 3, 2005, pp. 236–242., doi:10.1002/nau.20201.
Miller, J.M., et al. “Test-Retest Reliability of an Instrumented Speculum for Measuring Vaginal Closure Force.” Neurology and Urodynamics, vol. 26, no. 6, 2007, pp. 858–863., doi:10.1002/nau.20407.
Morin, M., Bourbonnais, D., Gravel, D., et al. (2004) Pelvic floor muscle function in continent and stress urinary incontinent women using dynamometric measurements. Neurourol Urodyn , 23: 668– 674.
Morin, Mélanie, et al. “Reliability of Dynamometric Passive Properties of the Pelvic Floor Muscles in Postmenopausal Women with Stress Urinary Incontinence.” Neurology and Urodynamics, vol. 27, no. 8, 2008, pp. 819–825., doi:10.1002/nau.20603.
Paul-Dauphin, A., et al. “Bias and Precision in Visual Analogue Scales: A Randomized Controlled Trial.” American Journal of Epidemiology, vol. 150, no. 10, 1999, pp. 1117–1127. doi:10.1093
Peschers, U. M., et al. “Evaluation of Pelvic Floor Muscle Strength Using Four Different Techniques.” International Urogynecology Journal and Pelvic Floor Dysfunction, vol. 12, no. 1, 2001, pp. 27–30., doi:10.1007/s001920170090.
Romanzi, Lauri J., et al. “Simple Test of Pelvic Muscle Contraction during Pelvic Examination: Correlation to Surface Electromyography.” Neurology and Urodynamics, vol. 18, no. 6, 1999, pp. 603–612., doi:10.1002/(sici)1520-6777(1999)18:63.0.co;2-h.



